Derrick Morton was skeptical about working for Kaiser Permanente’s Bernard J. Tyson School of Medicine. The Pasadena, Calif., school hadn’t yet opened to students when he was offered a job in early 2020, and it felt risky to work for such a new institution. But Morton, who is Black, was eventually sold by the medical school’s mission: to train doctors with a strong focus on diversity, equity, and inclusion and to dismantle health disparities.
After a short time as an assistant professor of biomedical science, however, Morton says it became clear that the reality didn’t live up to his “great expectations.” In a lawsuit filed Aug. 22, Morton alleges that Kaiser’s medical school discriminates against Black faculty, fostering a culture of “anti-Black animus” that is “so pervasive and chilling that [Morton] and his Black colleagues could not associate with each other or with Black students for fear of being blacklisted and rendered professionally non-viable.”
At least a dozen times between October 2020 and July 2021, Morton alleges that he complained to supervisors that Black employees were being discriminated against and treated unfairly, including through demotions, discipline, and efforts to “silence” those who spoke out. Morton claims that he personally experienced similar issues—including being appointed to a diversity, equity, and inclusion advisory committee that, he says, was stripped of authority and effectively made secondary to an outside consultant. Morton claims that the toxic work environment at Kaiser caused him to develop panic attacks and insomnia, and to seek out therapy for the first time in his life.
A spokesperson for the medical school said they were “surprised” by Morton’s complaint and “strongly disagree with the allegations and characterization of events” within it, but declined to provide further comment on the lawsuit because litigation is ongoing.
The spokesperson stressed that “addressing equity, inclusion, and diversity in medical education and health care is one of our primary objectives at the Kaiser Permanente Bernard J. Tyson School of Medicine.” They noted that the school recruits a diverse body of students and faculty; that anti-racism is woven throughout its curriculum; and that Black faculty members hold many leadership and committee positions at the school.
Morton isn’t the first ex-faculty member to sue Kaiser’s medical school. Last year, former instructor Dr. Aysha Khoury filed a complaint against the school, alleging that she’d been suspended and ultimately terminated—without warning or a satisfying explanation—after leading a classroom discussion on racism in medicine, drawing on her own experiences as a Black woman and physician. Prior to that incident, Khoury alleges she endured microaggressions related to her gender and race, including extra scrutiny and supervision of her work and being reprimanded for failing to greet a white male colleague. Khoury tells TIME she hopes her lawsuit will ensure that “nothing like what I experienced happens to another faculty member.” Both Khoury and Morton are seeking monetary damages as well as policy changes to prevent future discriminatory behavior.
In June, the National Labor Relations Board (NLRB), a federal agency that protects fair labor practices, filed a complaint on Khoury’s behalf. School representatives declined to comment on Khoury’s complaint and time at the school, citing ongoing litigation. Kaiser’s lawyers filed a motion for summary judgment in August, arguing that Khoury had not proven she faced racial or gender discrimination and that her case falls exclusively under the NLRB’s jurisdiction.
In interviews with TIME, more than half a dozen current and former faculty members said they consider racism to be a systemic problem at the new medical school despite its progressive veneer. And Kaiser isn’t alone. U.S. medical schools both new and old are struggling to live up to their stated goals around diversity and inclusion and cast off the long history of racism embedded in U.S. health care—problems too deeply entrenched for a few well-placed buzzwords to fix.
One of the guiding values of Kaiser’s medical school is “advocating for change in medical education, the profession, and the healthcare system”—a proclamation that underscores how deep-seated issues of racism and inequity are in American medicine.
Centuries ago, enslaved Black people were forced into medical research, at times withstanding procedures without proper pain medication so that white doctors could learn about the human body. Modern medicine was “built on bodies that were Black, enslaved, had no autonomy, were abused and misused,” says Dr. Rachel Bervell, who runs the Black ObGyn Project, an initiative dedicated to anti-racism in medicine.
That mistreatment didn’t end with slavery. During the infamous Tuskegee study, which began in the 1930s, researchers withheld syphilis treatment from hundreds of Black men so they could see what the disease did to the human body over time. And well into the 1900s, it wasn’t uncommon for doctors to perform procedures, particularly on patients of color, without informed consent, as in the well-known case of Henrietta Lacks, a Black woman whose cancerous cervical tissue was taken without her knowledge during a medical visit in 1951, and later formed the basis for lucrative biomedical research projects. Those are only two of many examples, and they’re not ancient history. Even today, studies show that people of color in the U.S. experience poorer health care than white Americans. That’s particularly true when they’re treated by doctors of a different race—which is likely, since 56% of practicing physicians in the U.S. are white.
A white coat isn’t a shield against racism, either. Many physicians of color report experiencing racism from patients and colleagues, studies show, and almost a quarter of medical students who identified as an underrepresented minority say they experienced race-based discrimination during medical school, according to one 2020 study of 27,500 graduates. About 4% of medical students who experience recurrent discrimination or mistreatment ultimately leave medical school, according to 2022 research—and students of color are disproportionately likely to fall in that category.
Inequality is baked into the very structure of modern medical education. In the early 1900s, the Carnegie Foundation commissioned education expert Abraham Flexner to assess the state of U.S. medical schools. Inspired by the German model for educating doctors, which pushed for the advancement of research and biomedical science, Flexner recommended shutting down schools with subpar facilities or underperforming research programs. Almost 100 medical schools closed in the wake of his review, including five of the seven dedicated to educating Black students. The Association of American Medical Colleges (AAMC) has since acknowledged the harm caused by the Flexner report, but its influence on medical education is still felt today—perhaps most painfully in the shortage of Black physicians in the U.S., who make up just 5% of the doctor workforce. Closed Black medical schools could have trained approximately 35,000 additional Black physicians by 2019, one study found.
Many of medicine’s forefathers held racist beliefs that bled into medical training—like the idea that race itself predisposes people to certain ailments, or the false belief that people of color feel less pain than white people. So-called “race-based medicine” has been discredited in recent years, and the AAMC recently introduced new tools for teaching and assessing competency in diversity, equity, and inclusion—but in many cases, the damage has been done.
Kaiser’s medical school aimed to address many of these long-standing problems. When it announced in February 2019 that it would soon start accepting applications for its first class, it was explicit about its mission: to train “diverse physicians to serve the needs of society.” It would offer free tuition to the first five graduating classes, in order to attract the right students regardless of their ability to pay.
It sounded like “a little slice of utopia,” says a current faculty member who asked to go unnamed for fear of retaliation. But for some faculty of color, working at the school has not lived up to the promise.
In 2017, Kaiser hired Victoria Richards, a pharmacologist with experience in medical school curriculum development who has since left the school, to help shape its academic programming before it opened. At first, she says, the school’s ethos seemed to match its stated mission. But very quickly, Richards perceived the school’s focus shifting toward becoming an elite research institution—just like other prestigious medical schools—and the diversity initiatives started to seem like distant priorities. “I became disillusioned and disappointed,” she says, “particularly as the dean was hired and brought in.”
That dean was Dr. Mark Schuster, a lauded pediatrician and former Harvard Medical School professor. At least on paper, Schuster shares the school’s values. An article he co-authored about the school’s founding, published in the journal Academic Medicine in 2020, uses the acronym “EID”—for equity, inclusion, and diversity—49 times. But as Richards saw it, Schuster brought with him what she calls a “Harvard mentality”—one that seemed to value prestige and traditional trappings of academic success above values Kaiser’s medical school claimed to hold sacred, such as training community-oriented physicians who could help eliminate socioeconomic disparities in health.
Kaiser representatives did not make Schuster available for an interview. But Dr. Lindia Willies-Jacobo, the school’s senior associate dean for admissions and equity, inclusion, and diversity, insists the administration’s commitment to those values has never wavered. “It’s work, and we are doing the work,” she says. “As a Black woman…I will boldly say that I have never before worked at a school that was, in fact, as diverse as our school.”

Khoury, however, has a different perspective. She says that none of the 50 students in each of Kaiser’s first two classes came from a historically Black college or university (HBCU). And in Richards’ opinion, instead of looking for well-rounded students from diverse backgrounds, Schuster and his team appeared to prioritize applicants with excellent test scores—a metric that notoriously favors white, higher-income students—who would make the school look good as it got off the ground. (Willies-Jacobo strongly disagrees with the notion that applicants were not evaluated holistically, and says some HBCU graduates were admitted but chose not to attend. Fourteen percent of students in Kaiser’s first class identified as Black, higher than the 2020 national number of 9.5%.)
A former employee with knowledge of the school’s internal demographic data also says Kaiser had difficulty retaining faculty and staff of color across roles. (From 2017 to 2021, 11 of 13 voluntary faculty resignations came from people of color, according to Khoury’s legal complaint.) But unflattering data about retention were never distributed throughout the school, says the former employee. “Any data that ran contrary to the narrative [the dean] was trying to create, he would dismiss,” the former staffer says.
Indeed, a current faculty member, who asked to go unnamed to avoid retaliation, says the leadership team created an “unsafe environment to even just ask difficult questions.” Those who critique decisions made by leadership risk professional consequences, including removal from committees and being passed over for promotions, several current and former faculty members say.
Those themes are echoed in Khoury’s legal complaint, which cites an email sent to administrators by a faculty member of color who argued the school’s commitment to anti-racism was superficial. “We are a racist institution, we are upholding the system of white supremacy that is at the core of our nation, but we do not have to be,” the faculty member wrote, according to an excerpt included in the complaint.
Willies-Jacobo declined to comment on other people’s statements about how they perceive the school, but strongly defended Kaiser’s commitment to diversity, equity, and inclusion. She says that members of the leadership team take diversity, equity, and inclusion training sessions and have held “listening sessions” where students, staff, and faculty can share feedback.
Tensions boiled over when Khoury was abruptly suspended, with little explanation, in the summer of 2020. “Here I am thinking that I have the permission to be all of who I am, and that that is appreciated,” Khoury says, looking back on the experience. “And for them to not even speak to me is so disabling, traumatic. It strips you of any identity.”
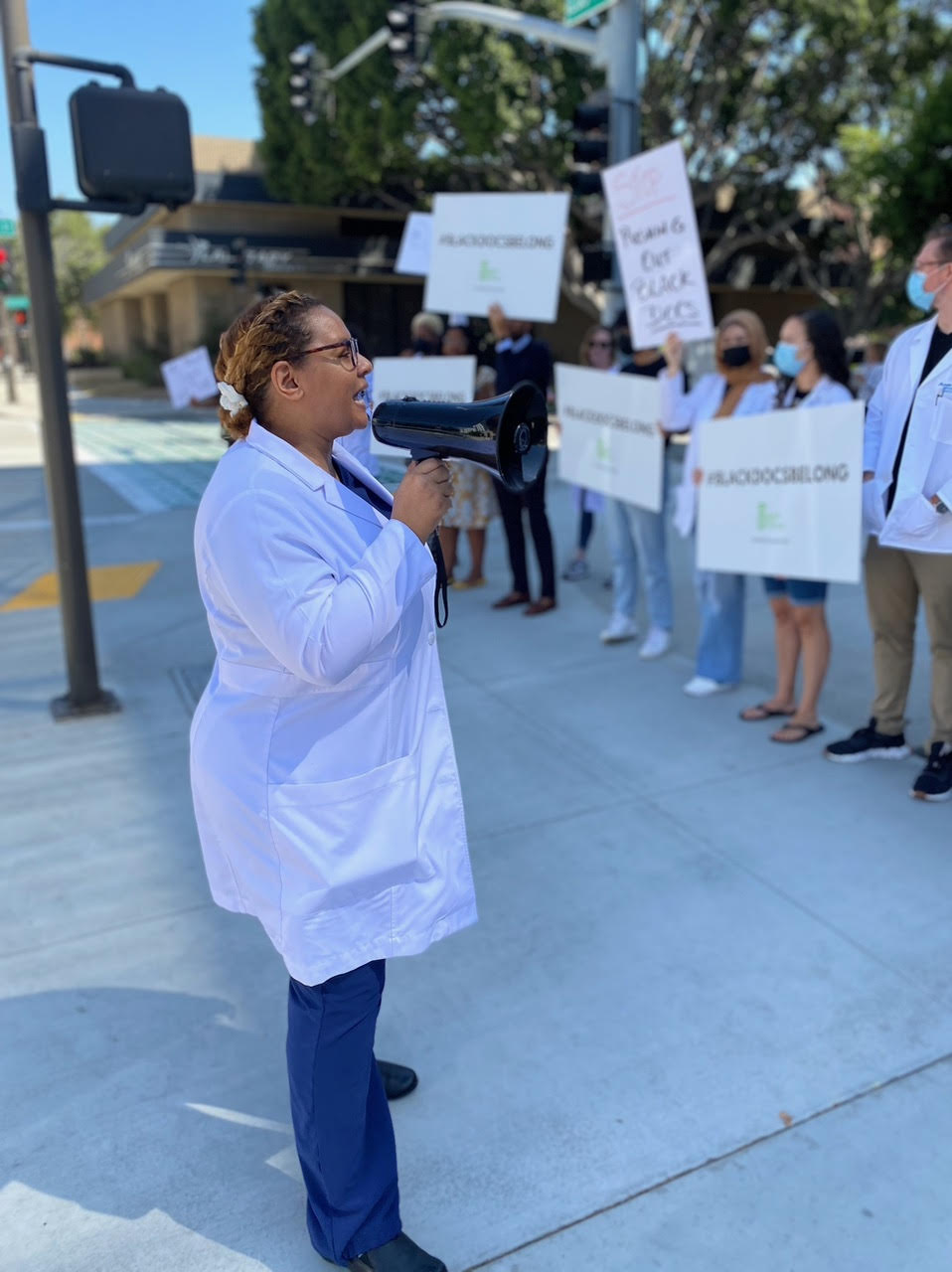
The incident was also traumatic for the wider Kaiser community. More than 90% of the first-year class signed a petition demanding Khoury’s reinstatement, according to a tweet from the account StudentsofKP, which describes itself as a group of students from the school’s class of 2024. Her case also sent ripples of fear through a faculty already on edge, some of her colleagues say. If an instructor could be suspended for leading a discussion about racism in medicine—at a school that had encouraged her to do just that—what else could be considered a fireable offense?
In the aftermath of Khoury’s departure, several Black students reached out to Morton and another teacher of color to talk about what had happened, Morton recalls. “‘We don’t think we can meet with you,’” he told them. “‘They may fire us.’” Morton’s legal complaint also alleges that a member of Kaiser’s leadership team implied in a meeting with Morton that his students could face consequences if they protested Khoury’s departure. Morton subsequently advised his students of color to partner with white students if they wanted to speak out against perceived racism on campus, believing the school to be more receptive to the white students’ concerns, the complaint says.
Less than a year after Khoury’s suspension, Morton took a job at another university and didn’t look back—despite a significant pay cut. The “culture and overt racism” at Kaiser, he says, “made it such that I couldn’t stay.”

Kaiser’s medical school opened in 2020, when racial issues were top of mind for the entire country. It had no history to overcome, no statues to tear down or buildings to rename. Yet to many, it’s still coming up short.
It’s far from the only medical school struggling to tackle issues of systemic racism and inequality. Schools both new and old are learning that breaking the mold created by centuries of medical racism is easier said than done. “We’re all cut from the same cloth,” a current Kaiser employee says of U.S. medical schools. “We just had the hubris and arrogance to claim that we could be different.”
In late 2021, Dr. Princess Dennar, who formerly ran a medical residency program at Tulane University, settled a lawsuit in which she alleged the school discriminated against doctors of color. A representative from Tulane said they could not comment on the lawsuit, but said Tulane has “embarked on a school-wide cultural change that places equity, diversity and inclusion at the center of our recruitment, training, teaching, research, operations and care.”
Dennar says she could not talk about her time at Tulane, but overall says she has never seen a medical institution totally overcome its racist foundations. “Medicine is a racialized system,” she says, and those historical roots keep inequities in place. “I would be hard-pressed to believe that there is an institution that exists today—if they still practice the same things they’ve been taught and built upon—that is absolved from having any forms of racism.”
But some schools—particularly those founded relatively recently—are trying. Charles Collier, an assistant dean at Quinnipiac University’s Frank H. Netter MD School of Medicine, has run a program that supports students from underrepresented backgrounds on their paths to medical school since 2012, two years after the school was founded. Collier says it was forward-thinking for the school to have such a program, especially a decade ago, but admits there have been “peaks and valleys” in its implementation.
He says he has faced resistance from colleagues who don’t see why minoritized students need more support than other prospective applicants—though that pushback melted away after the uprising that followed George Floyd’s murder in 2020, he notes. (In a statement, Dean Dr. Phillip Boiselle said the program has always had full institutional support.) Collier says there’s been sustained momentum since 2020, and the school recently hired an inaugural associate dean for equity, inclusion, and diversity—a promising sign, he says.
Frank Netter isn’t perfect, but Collier believes it is doing a better job at confronting inequality than most U.S. medical schools. That’s in large part, he says, because its students are motivated to effect change, forcing administrators to listen. Student pressure, he says, was the “catalyst” for hiring the new associate dean for equity, inclusion, and diversity. Boiselle agrees that student feedback has been “especially vital” in shaping Netter’s approach to diversity, equity, and inclusion, a process that he says will continue into the school’s second decade.
Similar battles are playing out at older schools, which have considerably more history to overcome. Harvard has been publicly reckoning with its historical ties to slavery, and that’s an ongoing process, says Dr. Joan Reede, dean for diversity and community partnership at Harvard Medical School. “Everyone acknowledges that we are not at the end of uncovering,” she says.
Still, Reede notes that Harvard Medical School has been engaged in diversity, equity, and inclusion efforts for more than 50 years, dating back to when a former dean in 1968 created a committee meant to help diversify the student body.
LaShyra Nolen, president of Harvard Medical School’s 2023 graduating class, says Harvard’s medical students and residents are widely committed to equity and anti-racism, but it can be hard to inspire the same enthusiasm from veteran figures in medicine. She points to a recent book written by Dr. Stanley Goldfarb, a former dean at the University of Pennsylvania’s medical school, called Take Two Aspirin and Call Me By My Pronouns: Why Turning Doctors Into Social Justice Warriors Is Destroying American Medicine, which she describes as specifically mocking her anti-racism advocacy. “As we’re making strides,” Nolen says, “we still have this old guard” that is resistant to change.
Nolen has been encouraged that Harvard now accepts EID work for senior thesis projects and factors it into faculty promotion assessments. Previously, she says, EID was often considered a “volunteer” commitment, rather than academically rigorous work.
That gets at a systemic problem. The medical education system relies heavily on standardized tests and other similarly one-dimensional performance metrics. Even though a growing number of undergraduate colleges are deemphasizing standardized test scores in part because of research suggesting they reinforce racist and culturally biased admissions processes, many medical schools continue to use them. Schools that try to do things differently—prioritizing hands-on learning over exams, accepting students with other valuable medical skills but not-so-great scores—risk producing doctors who can’t compare, at least on paper, to their competitors’ graduates.
Several current and former Kaiser medical school employees say the numbers-focused system partially explains what they see as the institution’s failure to live up to its anti-racism goals. The school is so new that it is still going through the process of accreditation, through which institutions must prove they meet the necessary standards for granting degrees. Since that process is crucial to the school’s future, current and former faculty members say leadership is making every effort to present an impressive facade to outsiders—even if it means glossing over internal culture and equity issues that don’t show up on an evaluator’s spreadsheet.
As of August, Kaiser has been granted preliminary accreditation by the Liaison Committee on Medical Education. It was also recently included on U.S. News & World Report’s list of the most diverse medical schools in the U.S. Willies-Jacobo acknowledges that the pressures of accreditation “are real.” But “having said that,” she continues, “I would say that we have pushed, and will continue to push, boundaries.”
Pushing boundaries within an existing system doesn’t go far enough, Dennar says. The entire health care system was built upon racist foundations, and she’d like to see a similarly ground-up approach to remaking it. Starting in medical schools, and continuing all the way through the current health care workforce, Dennar wants more emphasis on holistic patient care, better understanding of how race and health intersect, and stronger connections between clinicians and the communities they treat. She’s optimistic, but not delusional: “We have a lot of bandages being put on wounds, and the wound is still festering,” she says.
Despite everything, Khoury still wants Kaiser’s medical school to live up to its ideals; she believes the school, as described on paper, should and could exist. With “some significant humility, accountability, introspection, and dedication to anti-racism,” she thinks it can get there. Changes to the way it deals with racism on campus and commitment to transparency and academic freedom would be good places to start, she says.
But Khoury knows that work takes energy and dedication, and she fears that both may be in short supply at Kaiser. If efforts fall short, she’s afraid others will be lured to the school for the same reasons she was, only to be disappointed. “There’s a part of me that would rather them just change their mission,” she says. “That might be easier to do.”
- Tarana Burke: What 'Me Too' Made Possible
- Column: Youth Incarceration Harms America's Children. It's Time to End It
- What TIME's Newest Class of Next Generation Leaders Can Teach Us
- 14 Actually Good Books To Teach Kids About Climate Change
- Column: The Fate of the Amazon Rainforest Depends on the Brazil Election
- Lessons From a Half-Century of Reporting on Race in America
- What Happens If I Get COVID-19 and the Flu at the Same Time?
- A Year After Striketober, Employers and Labor Unions Aren't Getting Along